Spina Bifida : Understanding the Medical Aspects of Neural Tube Defect
Introduction:
Spina Bifida is a complex congenital condition characterized by the incomplete closure of the neural tube during fetal development. This condition affects the spinal cord and the surrounding structures, resulting in a range of physical and neurological impairments. In this blog, we will explore the medical aspects of Spina Bifida, including its etiology, clinical manifestations, diagnosis, and management. By gaining a deeper understanding of this condition from a medical professional perspective, we can provide comprehensive care and support to individuals with Spina Bifida.
Etiology:
Spina Bifida occurs when the neural tube, which develops into the brain and spinal cord, fails to close properly during early embryonic development. The exact cause of this condition is multifactorial, involving a combination of genetic and environmental factors. Folic acid deficiency during pregnancy has been identified as a significant risk factor for Spina Bifida. Other contributing factors may include genetic mutations, maternal diabetes, certain medications, and exposure to certain environmental factors.
Clinical Manifestations:
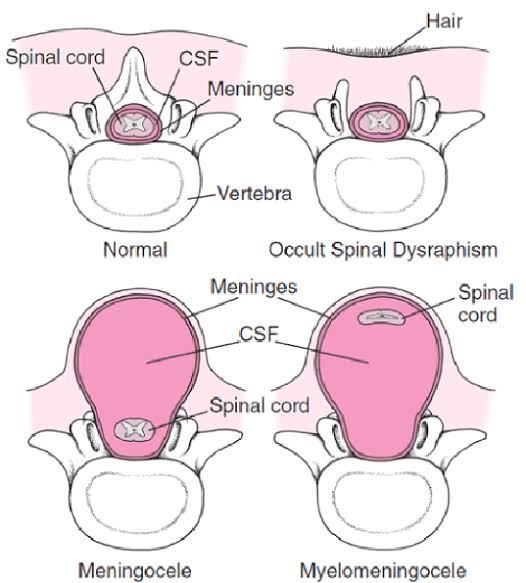
The clinical manifestations of Spina Bifida can vary widely depending on the severity and location of the spinal cord defect. The three main types of Spina Bifida are:
Spina Bifida Occulta: This is the mildest form, where the spinal cord and nerves are usually not affected. There may be a small gap or malformation in the vertebrae, often not visible externally.
Meningocele: In this type, the protective covering of the spinal cord, called the meninges, protrudes through the spinal defect, forming a fluid-filled sac. The spinal cord itself remains intact.
Myelomeningocele: This is the most severe form, characterized by a sac-like protrusion containing the spinal cord and its protective covering. The spinal cord is often damaged and may result in varying degrees of neurological impairment.
Neurological Impairments:
Individuals with Spina Bifida, particularly those with myelomeningocele, may experience a range of neurological impairments. These can include paralysis or weakness in the legs, loss of sensation, bladder and bowel dysfunction, and hydrocephalus (an excessive accumulation of cerebrospinal fluid in the brain). The severity of these impairments can vary greatly among individuals and may require lifelong management and support.
Diagnosis:
Prenatal screening, such as maternal serum alpha-fetoprotein (AFP) testing and ultrasound, can help identify the risk of Spina Bifida in the developing fetus. If an increased risk is identified, further diagnostic tests, such as amniocentesis or chorionic villus sampling, can be performed to confirm the diagnosis.
Postnatally, physical examination and imaging studies, such as ultrasound, magnetic resonance imaging (MRI), or computed tomography (CT) scans, can provide a more detailed evaluation of the spinal cord defect and associated abnormalities. Early diagnosis is crucial in initiating appropriate interventions and planning for the management of Spina Bifida.
Management and Support:
The management of Spina Bifida requires a multidisciplinary approach involving various healthcare professionals. A team consisting of pediatricians, neurosurgeons, orthopedic surgeons, urologists, physical therapists, occupational therapists, and psychologists work collaboratively to address the diverse needs of individuals with Spina Bifida.
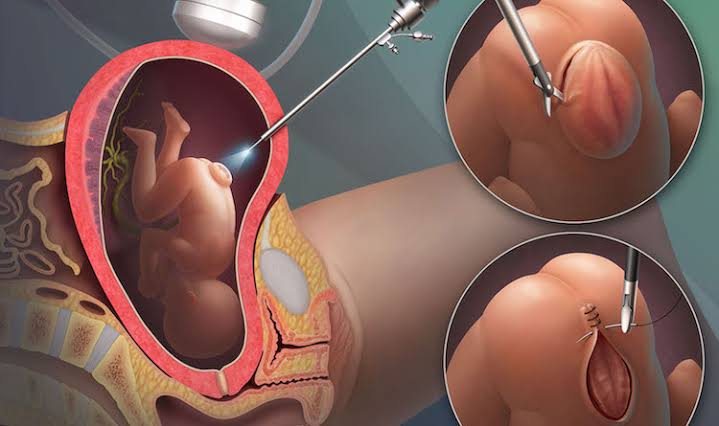
Surgical intervention is often necessary to repair the spinal defect and prevent further damage. Timing and extent of surgery depend on the type and severity of Spina Bifida. For individuals with myelomeningocele, early closure of the spinal defect is typically recommended to reduce the risk of infection and further neurological damage.
Physiotherapy plays a crucial role in promoting mobility, muscle strength, and functional independence. Occupational therapy focuses on enhancing fine motor skills, self-care abilities, and facilitating independence in daily activities. Additionally, assistive devices such as braces, wheelchairs, or orthotic devices may be prescribed to optimize mobility and support.
Individuals with Spina Bifida often require ongoing management of associated conditions such as hydrocephalus, bladder and bowel dysfunction, and orthopedic abnormalities. Regular follow-up visits, imaging studies, and consultations with specialists are necessary to monitor and manage these issues effectively.
Psychosocial support and counseling are essential components of comprehensive care for individuals with Spina Bifida and their families. Addressing emotional well-being, promoting positive body image, facilitating educational support, and fostering social integration are crucial in promoting the overall quality of life for individuals with Spina Bifida.
Conclusion:
Spina Bifida is a complex congenital condition that impacts the spinal cord and its surrounding structures. Understanding the medical aspects of Spina Bifida, including etiology, clinical manifestations, diagnosis, and management, allows healthcare professionals to provide comprehensive care and support. Through a multidisciplinary approach, early interventions, surgical repair, physiotherapy, and ongoing management of associated conditions, individuals with Spina Bifida can achieve optimal outcomes and lead fulfilling lives.








Comments
Post a Comment